On any given night in Las Vegas, the crowds show up for what has become one of the hottest shows in town. It’s “Menopause: The Musical” – 90 minutes of singing on a topic people used to just whisper about, from hot flashes to weight gain.
The show has been around for more than two decades, and when it first debuted, say producers Kathi and Alan Glist, people weren’t talking about menopause out loud. “It was called the ‘silent passage,'” said Kathi Glist, “because there was such a stigma, almost shame attached to it at that time.”
CBS News
Symptoms like hot flashes and mood swings usually start in what’s called perimenopause, the months or years leading up to menopause itself. And if you didn’t know that, you’re not alone.
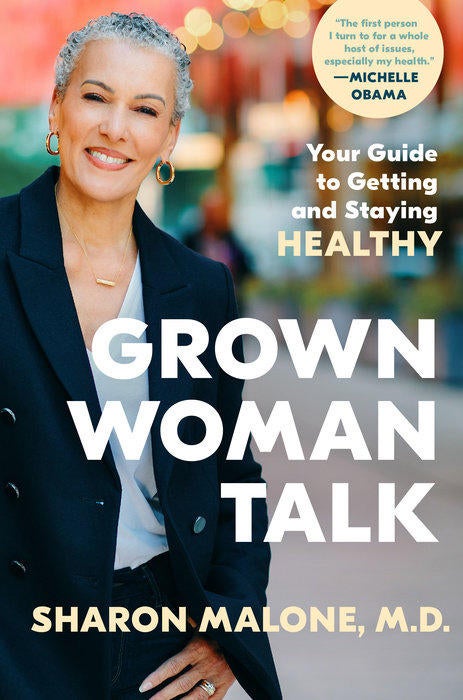
Dr. Sharon Malone is an OB-GYN, and an author who is trying to take the mystery out of menopause with a new book, “Grown Woman Talk: Your Guide to Getting and Staying Healthy” (Crown). She says most women do not know what to expect when it comes to menopause. “Most women have no idea when this whole perimenopause or menopausal transition starts,” she said.
And how long does it last? “That’s the $64,000 question,” Malone said. “Every woman is different, but the average is in the range of years, not months.”
Crown
There are new treatments for menopause symptoms. But the most common is hormone replacement therapy, or HRT, a cocktail of different types of estrogen to put back what the body isn’t making enough of. Starting in the 1940s, that estrogen mixture came in pill form, sold under the clinical-sounding name Premarin.
And you might not believe where the name comes from: “Pregnant mares’ urine,” said Malone. “Horses, you can image, put out a lot of urine. And as long as you keep the mares pregnant, you have an almost inexhaustible supply.”
And until 2002, it seemed that there was an inexhaustible supply of menopausal women lining up for hormone replacement therapy. Malone said, “Estrogen is not the only answer. But it is the most effective answer. For women who are symptomatic – and by that I mean women who have, you know, hot flashes, night sweats, sleeplessness, mood swings, and the list goes on and on – nothing treats those symptoms better than estrogen therapy. And that’s period, end of sentence.”
By the early 2000s, an estimated six million post-menopausal women were taking hormones. But then, HRT got a black eye. During the 1990s, a government study called the Women’s Health Initiative was investigating a link between estrogen and a decrease in heart disease. But the study’s directors found something else, and on July 9, 2002 they dropped a bomb:
Malone said, “They did not find the expected benefit in the decrease in the risk of cardiovascular disease, which was troubling in and of itself. But more importantly, there was a 26% increase in the risk of breast cancer. And when they reported out the increased risk in breast cancer, it was almost game, set, and match for the hormone therapy market.
“Women are more afraid of breast cancer than they are of cardiovascular disease, despite the fact that more women die of cardiovascular disease than breast cancer, at any age,” said Malone.
But the headlines didn’t tell the whole story. A closer look at that study showed that for most women the risk of breast cancer from hormone therapy is actually very low, and that for younger women HRT does lower the risk of cardiovascular disease.
Still, it seems most women only heard the bad news, and started throwing their hormone pills down the drain. “They’re like, ‘I’m not takin’ this, I don’t care how I feel, I’m not gonna do this, because you are increasing my risk of breast cancer,'” Malone said.
What’s more, the news also had a chilling effect on women’s health issues in general, said Jennifer Weiss-Wolf from the Brennan Center for Justice at NYU Law School. “Menopause became absolutely deprioritized,” she said. “Doctors stopped learning about it. Medical schools stopped teaching about it. And the government stopped funding federal research for it. So, we found ourselves in an information vacuum that persisted all the way up until this new chapter where people have started demanding change.”
Things are changing. There are several bills addressing menopause education and treatment working their way through Congress; and just last month, President Biden signed an executive order authorizing millions for women’s health research, including for menopause.
And at the grassroots level, women are making change by talking about “the change.” Recently in San Diego there was a gathering known as “Menopause Mondays” – a little wine, a few laughs, and a whole lot of information about menopause.
The cheerful emcee is Ellen Dolgen, who started holding these seminars 20 years ago after a bad experience with her own menopause. “My goal is to educate women,” she said. “My motto is, suffering and silence is out, and reaching out is in. I don’t want anyone to go through what I went through because I was completely uneducated. And it shouldn’t be, it’s not necessary.”
CBS News
And there is an information gap. Some of the women “Sunday Morning” talked with were actually dealing with perimenopause, and just didn’t know it. One woman said, “Turns out after this function I realize that I do have symptoms. I’m just passing it off as life – like, I can’t sleep, I’ve just been busy, brain fog, I’m just juggling a lot of things.”
Dolgen has hosted these parties in more cities than she can count, and she says there’s no end in sight. To her, menopause is having a moment. “I think it’s kind of chic right now,” she said. “Like, I’m wearing my menopause right now and I think I’m pretty damn chic!”
And so the big news flash here might be ignorance about menopause is out, suffering is out, treatment is in.
Dr. Malone said. “I want women to understand that, you know, menopause is inevitable. If you have ovaries, you will go through menopause, whether you have symptoms or not. The message is that menopause is inevitable; suffering is not.”
Smith asked, “Do you think women still have this idea that we are supposed to suffer?”
“We have sort of incorporated the language of suffering into the entirety of women’s existence,” Malone said. “We have to get used to the fact that it’s okay to want to feel better.
“Why do we as women not have the ability to make decisions for ourselves without feeling guilty? Put yourself first to say that, ‘My quality of life is important.’ What’s wrong with that?”
READ AN EXCERPT: “Grown Woman Talk” by Sharon Malone, M.D.
For more info:
Story produced by John D’Amelio. Editor: Steven Tyler.

 Latest Breaking News Online News Portal
Latest Breaking News Online News Portal