
The most common type of gynecologic cancer in the U.S. has been on the rise in recent years — and there’s no standard screening for it.
Uterine cancer will affect about 66,200 women in 2023 in the U.S. — and around 13,000 will die from the disease, per the American Cancer Society (ACS).
“While we are seeing a downward trend in overall cancer cases, uterine cancer is one of the few types where we’re seeing an upward trend,” said Dr. Brian Slomovitz, director of gynecologic oncology and co-chair of the Cancer Research Committee at Mount Sinai Medical Center in Miami Beach, Florida, in an interview with Fox News Digital.
CHEMICAL HAIR-STRAIGHTENING PRODUCTS MAY INCREASE UTERINE CANCER RISK: NIH STUDY
“We’re anticipating that the number of deaths in the United States due to uterine cancer is soon going to outnumber the deaths due to ovarian cancer,” he added.
To help raise awareness, the International Society of Gynecologic Cancer announced the first-ever Uterine Cancer Awareness Month in June.

Dr. Brian Slomovitz is director of gynecologic oncology and co-chair of the Cancer Research Committee at Mount Sinai Medical Center in Miami Beach, Florida. He also serves as chair of the Uterine Cancer Awareness Month initiative. (Mount Sinai Medical Center)
Slomovitz — who also serves as chair of the Uterine Cancer Awareness Month initiative — spoke to Fox News Digital about the state of uterine cancer and what women need to know.
Uterine cancer and endometrial cancer: What’s the difference?
The terms “uterine cancer” and “endometrial cancer” are often used interchangeably, but there is a difference, Slomovitz said.
A vast majority of these types of cancers occur in the outer and inner layers of the uterus, known as the endometrium — hence the term “endometrial cancer.”
About 4% to 5% of the cancers occur in the muscle of the uterus. These are known as uterine sarcomas.
NEW YORK DOCTORS USE ARTIFICIAL INTELLIGENCE TO BETTER DETECT BREAST CANCER
“Sarcomas are aggressive diseases with a tremendously high death rate,” Slomovitz explained. “But all of them fall in the category of uterine cancers.”
The biggest risk factor of all
Obesity is the biggest risk factor for uterine cancer, Slomovitz said.
“Fat tissue increases the amount of estrogen in the body, and endometrial cancer is a hyper estrogenic,” he explained. “It stimulates the lining of the uterus to the point of uncontrolled proliferation into cancer.”

“There are some game-changing studies coming out, as we try to fill this unmet need to help our patients live longer,” said Dr. Slomovitz, shown here. (Mount Sinai Medical Center)
Overweight women (with a body mass index of 25 to 29.9) have twice the risk of developing uterine cancer as women at a healthy weight, the ACS website states.
Obese women (BMI of 30 or higher) have three times the risk.
Those with diabetes, which is closely related to obesity, are also at a higher risk.
Obesity and age are two of the biggest risk factors for uterine cancer.
A less common risk factor could be polycystic ovarian syndrome (PCOS), which is a hormonal disorder that can lead to enlarged ovaries and the formation of cysts.
PCOS leads to elevated estrogen levels and lower progesterone levels, which can raise the risk of endometrial cancer, according to the American Cancer Society (ACS) website.
Some hereditary syndromes can make women more susceptible to uterine cancer.

Dr. Slomovitz has worked in the field of gynecologic oncology for over 20 years; he currently serves as director of gynecologic oncology and is co-chair of the Cancer Research Committee at Mount Sinai Medical Center in Miami Beach. (Mount Sinai Medical Center)
“One of those is Lynch syndrome, which was often associated with colorectal cancer,” said Slomovitz.
“We know that half the women who develop cancer from Lynch syndrome develop endometrial cancer.”
Age is also a risk factor, as most patients are diagnosed in their 50s and 60s, the doctor said.
“The increase in cases may be due to obesity, but we’re also seeing longer life expectancy,” he noted. “The older people get, the more likely that they are to get endometrial cancer, obviously.”
Symptoms and screening
While other cancers have specific, recommended screenings — such as mammograms for breast cancer and colonoscopies for colorectal cancer — there are no pre-symptomatic screenings for uterine cancers, per the Centers for Disease Control and Prevention (CDC).
The Pap smear (Pap test) checks for cervical cancer and precancerous cells in the cervix, but does not screen for uterine cancer.
CERVICAL CANCER: WHAT ARE THE SIGNS AND SYMPTOMS?
The most common sign or symptom of uterine cancer is abnormal bleeding, Slomovirz said.
“Most uterine cancer patients have postmenopausal bleeding as an early sign or symptom — however, that’s not the case for everyone,” he said.
In premenopausal women, it can be more difficult to determine what constitutes “abnormal” bleeding, the doctor noted.
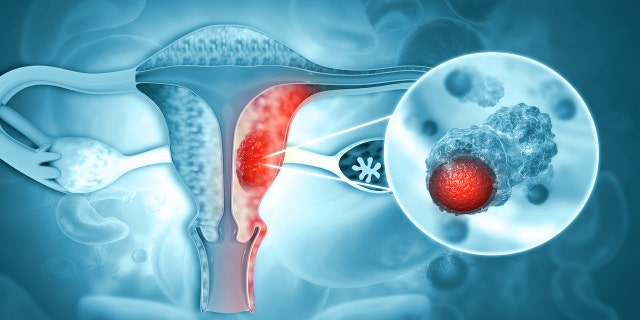
Uterine cancer will affect some 66,200 women in the U.S. in 2023 — and around 13,000 women will die from it, per the American Cancer Society. (iStock)
“They shouldn’t just assume it’s changes in their menstrual cycle,” he said.
In the absence of a formal screening process, Slomovitz stressed the need to recognize symptoms and take quick action.
“We need to better educate patients to come see their doctors sooner if they have symptoms,” he told Fox News Digital.
“We need to better educate patients to come see their doctors sooner.”
In addition to bleeding, other symptoms may include pelvic pain or pelvic pressure.
TWO NEW CANCER PILLS SHOW ‘UNPRECEDENTED’ RESULTS IN BOOSTING SURVIVAL RATES AND PREVENTING RECURRENCE
“We always tell people that if they have symptoms that are worsening or if they persist after 10 to 14 days, they should come in to see their doctor just to make sure everything’s OK,” Slomovitz said.
“We’re still seeing a large number of patients who are diagnosed with advanced and recurrent disease.”

“We need to better educate patients to come see their doctor sooner if they have symptoms,” said Slomovitz. (iStock)
The diagnosis process typically starts with an ultrasound to take images of the uterus, followed by a tissue biopsy — either to diagnose or rule out the disease, said Slomovitz.
In cases of advanced cancer, patients will usually get additional tests — such as chest X-rays, CT scans, MRIs or PET scans — to determine if the disease has spread.
“It traditionally spreads through the lymphatic system, which means lymph nodes can be enlarged,” Slomovitz explained. “It can also spread to the liver or the lungs through the blood system.”
“Eighty percent of women are cured with a hysterectomy.”
In patients who have had endometrial cancer in the past, a gynecologic oncologist will instruct them that for any future symptoms, recurring cancer must be ruled out.
“They’re cancer patients — so even in the non-specific symptoms, it’s worthy of seeing their oncologist again to make sure it’s not coming back,” Slomovitz said.
Treatment options: ‘An unmet need’
In women who are diagnosed with uterine cancer, one of the first steps is usually a hysterectomy, which is the removal of the uterus.
“Eighty percent of women are cured with a hysterectomy,” Slomovitz said.
To further minimize risk, the doctor said medical professionals will often do lymph node sampling as well to make sure the cancer hasn’t spread.
“But for the additional 20% of patients who have advanced or recurrent disease, systemic therapies are needed,” he said. “We need to do better with treatment options for uterine cancer.”
For these aggressive cases, the systemic therapies have been chemotherapy or hormonal therapy, which uses progesterone to slow down tumor growth.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
This year, Slomovitz said, some breakthrough studies have shown that immunotherapy can be given in the first-line management of the disease.
Immunotherapy treatments work by helping the immune system to slow, stop or destroy cancer cells. It’s shown to be effective for lung cancer, oral cancer and melanoma, the doctor pointed out.

Symptoms of uterine cancer include abnormal bleeding and pelvic pain. (iStock)
At the American Society of Clinical Oncology conference in May 2023, researchers presented promising results for a new class of drugs called antibody-drug conjugates (ADCS), a targeted therapy for treating cancer, Slomovitz said.
Health professionals are trying “to fill this unmet need to help our patients live longer.”
Future studies will continue to look at these types of targeted drugs.
“One of my career goals is to use immunotherapy and targeted therapy to eliminate the need for chemotherapy and its associated toxicities and side effects,” Slomovitz said.
CLICK HERE TO GET THE FOX NEWS APP
Another “groundbreaking” advancement Slomovitz is particularly excited about is molecular classification, which divides uterine cancers into four different subtypes — thus allowing for more precise, personalized treatment options.
“We’re in a very exciting time,” he said. “There are some game-changing studies that are coming out, as we try to fill this unmet need to help our patients live longer.”

 Latest Breaking News Online News Portal
Latest Breaking News Online News Portal




